In Garut, pregnant women can access health services relatively easily. Yet, the number of maternal deaths is the third highest in West Java, the province with the highest population and highest burden of maternal deaths in Indonesia.
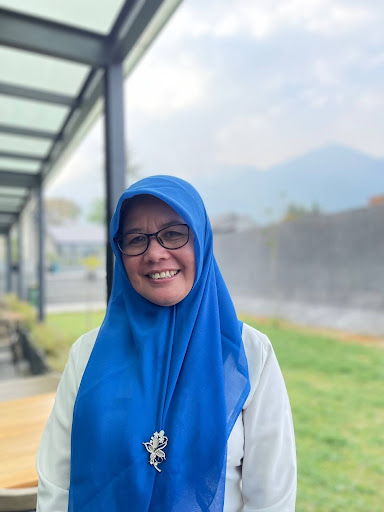
Garut District has 2.67 million population with more than 55,000 pregnant women annually. In 2023 alone, Garut recorded 60 maternal deaths and 320 neonatal deaths. "In Garut District, it is still high, yes, in terms of the number of maternal deaths... This is something that we must really pay attention to, so that we can immediately reduce maternal and infant mortality," said dr. Leli Yuliani, MM, Head of Garut District Health Office.

According to dr. Leli Yuliani, Head of Garut District Health Office, Garut has implemented a number of programmes to address maternal mortality including services for high-risk pregnant women.
(Photo: UNFPA/Rahmi Dian Agustino)
UNFPA and the Ministry of Health, supported by Australia’s Department of Foreign Affairs and Trade (DFAT), are implementing a pilot project in Garut to strengthen maternal health care, and ultimately, reduce maternal mortality.
Gaps in quality
The BEmONC in Puskemas Tarogong serves about 30 childbirths per month, below the international standard of 50 deliveries per month.
(Photo: UNFPA/Rahmi Dian Agustino)
The Ministry of Health has made access to quality Emergency Obstetric and Newborn Care (EmONC) a priority for the reduction of maternal mortality in Indonesia. Garut District was selected as the location of the pilot programme to redesign the health system to optimise EmONC facilities, with a potential scale-up at national level.
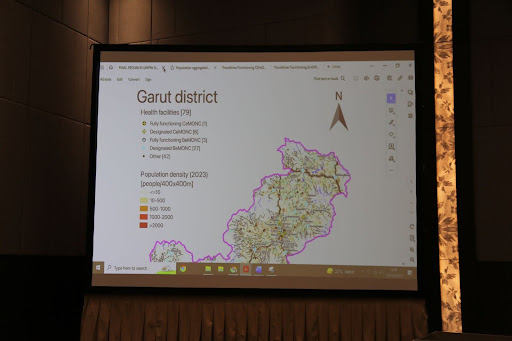
Garut has 67 public health centers (puskesmas), 30 of which provide basic emergency obstetric and newborn care (BEmONC). And out of seven hospitals, one provides comprehensive emergency obstetric and newborn care (CEmONC), the RSUD Slamet Garut in Garut city.
In other words, Garut has more than enough EmONC facilities required to serve the population. So why do mothers in Garut still face risks of preventable maternal deaths?
"This is a highly extraordinary assignment for us in Garut because at the 67 public health centers in 42 sub-districts, our target is to serve approximately 51,844 pregnant mothers,” said Sri Prihatin, S. Tr. Keb, MMKes from the Garut District Health Office.
Sri Prihatin found that, in addition to EmONCs, maternal and perinatal mortality audit, surveillance, and response (MPDSR) has also been useful for maternal mortality reduction. “It has provided guidelines for us to move forward.”
(Photo: UNFPA/Rahmi Dian Agustino)
There are gaps in the quality of care and facilities that need to be addressed urgently. While Garut has midwives working at EmONC facilities, the number of childbirths handled there is below the international standard of a minimum of 50 deliveries per month at each EmONC.
“The 12 midwives serving at the BEmONC do not work full time at the facility. There are village midwives and midwives who implement other programmes like child growth, adolescent health, or traditional health, or those who work in management,” Ita Kurnia, a midwife at Puskesmas Tarogong, one of the priority BEmONC facilities in Garut, explained.

For midwife Ita Kurnia, assisting safe childbirths is the highlight of her job. “The most memorable moments are when we see the family smiling joyfully.”
(Photo: UNFPA/Rahmi Dian Agustino)
According to Ita, the double responsibilities that midwives bear at the public health centers affect their ability to provide the best service for their pregnant mother patients. Midwife Ita also emphasized on the need for capacity building. “Our challenge lies in the human resources… If we focus on the BEmONC services, we would be more prepared to treat patients,” she said. “And not all midwives at the BEmONC have been trained in emergency services. So the support we need from the Health Office and the Ministry of Health is fulfilling human resources requirements since childbirth services need six hands. We need three persons in every shift so we can provide services 24 hours seven days,” she elaborated. “And there are tools and equipment that we do not have yet.”
The Garut District Health Office and the Ministry of Health agree that improvements in the EmONC facilities must be prioritized.
“What we must do is improve the effectiveness and efficiency of the BEmONC facilities so that they can provide optimal emergency services for pregnant mothers and newborn babies,” dr. Leli Yuliani, MM, Head of Garut District Health Office, affirmed. “We need to focus on training the human resources and strengthening the infrastructure.”

Addressing risk factors before pregnancy is also important to reduce complications during pregnancy and childbirth, according to Dr. Laila Mahmudah of the Ministry of Health.
(Photo: UNFPA/Rahmi Dian Agustino)
"What we need to do now is ensure that the BEmONCs and CEmONCs function as we expect... including ensuring that the human resources who provide the services at the BEmONCs have good competence, confidence, and capacity to manage emergency cases," Dr. Laila Mahmudah, Head of Maternal and Neonatal Working Group, Directorate of Nutrition and Maternal and Child Health of Ministry of Health, echoed dr. Leli’s statement.
Gaps in accessibility still high
Garut District has 2.67 million population with more than 55,000 pregnant women annually. In 2023 alone, Garut recorded 60 maternal deaths and 320 neonatal deaths.
(Photo: UNFPA/Rahmi Dian Agustino)
While Garut city offers the ease of access and abundant options of health facilities, southern Garut has geographical challenges that serve as a barrier to access. South Garut has only one hospital, the provincial hospital RSUD Pameungpeuk. And people in South Garut live in remote villages in South Garut, which means they have to go extra lengths to get to BEmONC facilities in the area.

Midwife Siti Qodariah pleaded for special attention for pregnant women and midwives in remote South Garut who face extra challenges in accessing and providing services.
(Photo: UNFPA/Rahmi Dian Agustino)
“The BEmONC we have in South Garut is different… from the geographic condition. The distance from the villages is really far and the roads are steep,” said Siti Qodariah, the midwife who is in charge of the BEmONC at the Cisewu Puskesmas in South Garut. “Sometimes they are not accessible by motor vehicles so the patient has to be carried by their family members… a patient can spend three hours and Rp 400,000 one way just to rent a car to reach the facility.”
“I hope that there is special attention for South Garut. Since our location is remote, we need to be extra careful in providing services, and put extra efforts,” Midwife Siti Qodariah said. “I am also grateful that Puskesmas Cisewu is a priority for improvement and capacity building… and that the Pameungpeuk hospital is now an EmONC facility so that we can get there within 2,5 hours as opposed to four hours to the hospital in Garut city.”

Meily Arovi Qulsum of the Ministry of Health hoped that capacity building is also provided for non-BEmONC public health centers not only in Garut and West Java, but also in other provinces with high maternal and neonatal mortality rates.
(Photo: UNFPA/Rahmi Dian Agustino)
According to Meily Arovi Qulsum from the Directorate of Quality and Accreditation of Healthcare Services of the Ministry of Health, the RSUD Pameungpeuk in South Garut needs strengthening in order to provide the best services. “We need blood services and OB/GYN doctors on standby as we still have a limited number of OB/GYN specialists in Garut District. We also need more capacity building for human resources,” she affirmed.
Addressing the gaps through data driven prioritisation

The prioritisation workshop in Garut was attended by midwives, doctors, and heath office staff.
(Photo: UNFPA/Rahmi Dian Agustino)
To improve the availability and quality of EmONC services, the Ministry of Health decided to optimise its network of EmONC facilities by implementing UNFPA’s approach of focusing efforts in a few health facilities while keeping a good coverage of the population within two hours of travel time.
During a prioritisation workshop in Garut in October 2023, midwives, doctors, and the Health Office staff participated in a prioritisation exercise supported by advanced mobile and global positioning system (GPS) technologies to address the social, transportation, and financial barriers. The approach uses geospatial intelligence systems (GIS), which are computer systems designed to collect, organise, manage, display and analyse geographically localised data.
Throughout the prioritisation exercise, GIS was used in the development of thematic maps showing the geographical distribution of indicators, location of health facilities, and spatial analyses combined with data from the health sector and other areas such as land planning, environment, and infrastructure. Supported by UNFPA and University of Geneva experts, the analysis generated accessibility maps that allowed Garut district to prioritise 12 out of 38 health facilities without compromising the coverage and accessibility.
“The prioritisation workshop was a really good learning experience for us working at the national level. For three days, we learned how to implement the guidelines that are being developed so that we can see the feasibility of the said guidelines. We also learned of the implementation steps to select the BEmONCs so that we can agree on the prioritisation of the BEmONCs to be developed,” said Dr. Laila. “It will also be useful for the development of BEmONCs and CEmONCs in Garut district, to inform our future BEmONC planning at the national level.”
In Garut district, the impact is even more immediate. “After the prioritisation we can focus our resources on ensuring the facilities are functional and ensuring the referral system works,” said dr. Leli, optimistically.
Collaboration need to end maternal mortality

In Indonesia, a mother dies every hour due to complications from pregnancy and childbirth. Midwives are the backbone of maternal health systems that provide care with care, supporting childbearing women and their newborns, and ensuring safe birth for families in remote and hard-to-reach communities.
(Photo: UNFPA/Rahmi Dian Agustino)
At national level, the Ministry of Health implements 11 priority programmes that consist of community empowerment, public awareness raising, strengthening of first level and advanced level health facilities (FKTP and FKTRL), and the Maternal and Perinatal Death Surveillance and Response System (MPDSR). UNFPA supports the Ministry of Health through technical assistance and capacity building for improving health management information systems, as well as evidence to inform policy making to end preventable maternal mortality.
“Our collaboration with UNFPA has really helped us, especially in addressing maternal mortality and strengthening emergency obstetric and newborn care services. I hope in the future we can prioritize interventions in border, island, and remote areas that might need different approaches compared to urban areas,” Dr. Laila said.
“In the future, I hope that all stakeholders from ministries and institutions collaborate well in reducing maternal and infant mortality rates, so that the national programme does not only belong to the Ministry of Health but becomes one of the national priorities,” Meily added.
With collaboration at all levels, the enormous task of ending maternal mortality in Garut, and ultimately, in Indonesia, is feasible. After all, maternal health is the foundation of the nation’s health.
“One of the indicators of the Human Development Index is health. And we know one of the health indicators is life expectancy, which is really impacted by maternal and neonatal mortality. So to improve the quality of our human resources, mothers and babies must be healthy,” Sri affirmed.
Rahmi Dian Agustino, Communications Analyst
Sandeep Nanwani, Reproductive Health Programme Specialist


